Revolutionizing Outpatient Cardiac Care with AI-ECG
AI is revolutionizing ECG interpretation in outpatient care, offering rapid, accurate, and scalable cardiac diagnostics, especially in remote areas.
Artificial Intelligence Transforms ECG Interpretation in Outpatient Care
The use of artificial intelligence (AI) in electrocardiogram (ECG) interpretation is rapidly changing how cardiac conditions are detected and managed in outpatient settings. Recent studies and clinical trials confirm that AI-powered ECG analysis—primarily using deep learning (DL) and convolutional neural networks (CNNs)—can match or even exceed the diagnostic accuracy of human experts, offering faster, more consistent, and potentially more accessible cardiac care outside the hospital. This technological leap is especially significant for primary care clinics, community health centers, and remote areas where access to cardiology specialists is limited.
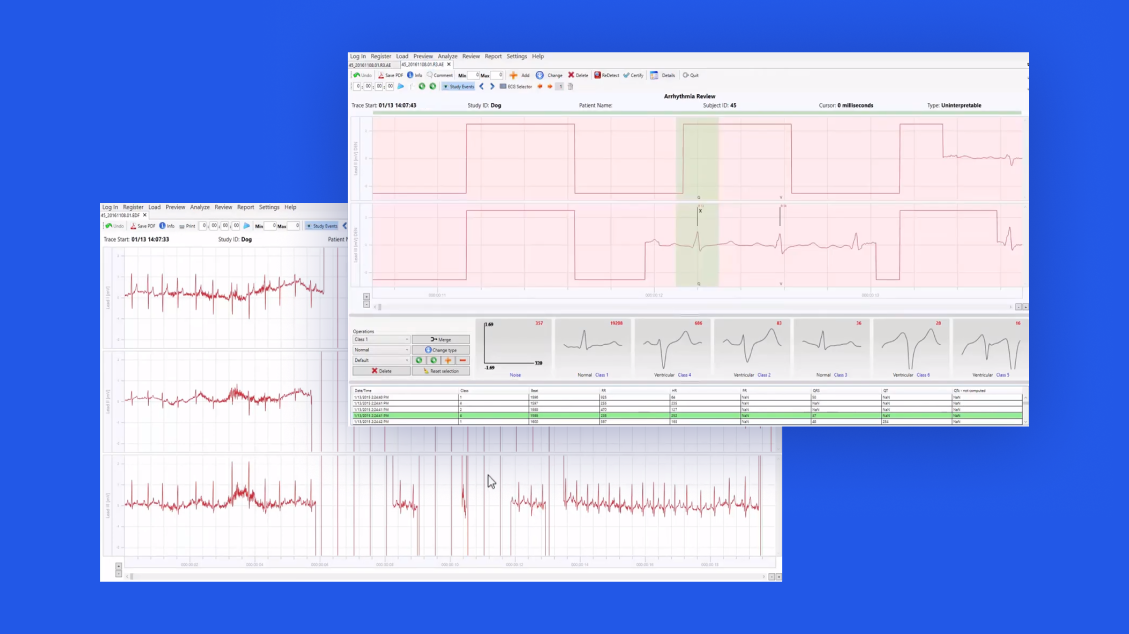
How AI Interprets ECGs
AI-enabled ECG interpretation relies on machine learning models trained on vast datasets of labeled ECG tracings. These models learn to recognize subtle patterns indicative of arrhythmias, ischemia, hypertrophy, and other cardiac abnormalities that may be missed by the human eye or in high-volume, routine screenings. The most advanced systems use 12-lead ECGs, the standard in clinical practice, and can process results in seconds—far faster than manual interpretation.
- Deep Learning Models: CNNs, a type of deep learning architecture, are particularly effective for image-based data like ECGs. They automatically extract features from raw ECG signals, reducing reliance on pre-defined rules or human feature engineering.
- Performance Metrics: AI models have demonstrated diagnostic accuracy rates between 75% and 85%, comparable to or better than emergency physicians, whose accuracy in high-stress scenarios typically ranges from 70% to 80%. Some studies report AI models achieving cardiologist-level performance, with certain systems outperforming human experts in specific tasks.
- Beyond Arrhythmias: While much attention has focused on arrhythmia detection (especially atrial fibrillation), AI is also being applied to predict other conditions, such as obstructive sleep apnea, directly from the ECG.
Clinical Applications and Workflow Integration
AI is not just a theoretical advance—it is already being integrated into outpatient workflows. For example, a sequential AI-ECG diagnostic protocol has been tested for opportunistic atrial fibrillation (AF) screening. This two-stage approach first applies a single-ECG AI model at the initial visit; if AF is not detected, a serial-ECG AI model is used after a short follow-up interval. This protocol achieved an area under the receiver operating characteristic curve (AUROC) of 0.908, with 88.1% sensitivity and 78.7% specificity. Importantly, it maintained a high negative predictive value (98.4%), meaning it reliably rules out AF in low-risk patients, while improving positive predictive value with longitudinal confirmation.
- Screening and Early Detection: AI-ECG tools enable large-scale, cost-effective screening for silent or paroxysmal conditions that might otherwise go undiagnosed until complications arise.
- Decision Support: These systems can flag abnormal recordings for further review by a clinician, reducing workload and potentially decreasing diagnostic delays.
- Remote and Underserved Areas: In regions with limited access to cardiologists, AI-powered interpretation can serve as a first-line diagnostic tool, ensuring timely triage and referral.
Evidence and Validation
Recent research highlights both the promise and the challenges of AI in ECG interpretation:
- Large-Scale Studies: Models trained on datasets exceeding two million ECGs have demonstrated superior diagnostic accuracy compared to human experts for certain conditions.
- Limitations: Current systems face challenges such as data collected from single centers, class imbalance in training datasets, and lack of electrophysiological validation, which may limit generalizability. Prospective, multi-center trials are needed to confirm real-world performance and cost-effectiveness.
- Regulatory and Ethical Considerations: As AI tools move into clinical use, issues of regulatory approval, liability, data privacy, and algorithmic transparency must be addressed to ensure patient safety and trust.
Industry Impact and Future Directions
The integration of AI into ECG interpretation is part of a broader trend toward AI-driven decision support in medicine. Companies and health systems are investing heavily in these technologies, seeing potential not only for improved outcomes but also for operational efficiencies and cost savings. For example, AI can prioritize ambulatory monitoring for patients most likely to benefit, optimizing resource allocation.
- Commercial Platforms: Several companies now offer FDA-cleared AI-ECG interpretation software, though widespread adoption in outpatient settings is still in early stages.
- Research Frontiers: Ongoing work focuses on expanding AI’s capabilities to predict a wider range of cardiac and non-cardiac conditions, personalize risk assessment, and integrate with electronic health records for seamless clinical workflow.
- Global Health Implications: In low-resource settings, AI-ECG tools could democratize access to high-quality cardiac diagnostics, bridging gaps in healthcare equity.
Context and Implications
The adoption of AI for ECG interpretation in outpatient care represents a paradigm shift in preventive cardiology. By enabling rapid, accurate, and scalable analysis of ECGs, AI has the potential to reduce undiagnosed cardiac disease, improve outcomes, and lower healthcare costs. However, successful implementation requires addressing technical, regulatory, and ethical challenges, as well as ensuring that these tools complement—not replace—clinical judgment.
As the evidence base grows and technology matures, AI-ECG interpretation is poised to become a standard component of outpatient cardiac care, transforming how millions of patients worldwide are screened, diagnosed, and managed for heart disease.



