AI Enhances Prediction of Hospital Stays Post-GI Surgery
Discover how machine learning predicts prolonged hospital stays after GI surgery, enhancing patient care and resource management.
AI Enhances Prediction of Hospital Stays Post-GI Surgery
Researchers have developed a machine learning-based prediction model to identify patients at risk of prolonged length of stay (LOS) following laparoscopic gastrointestinal (GI) surgery. This model, derived from a secondary analysis of the FDP-PONV trial, represents a significant advancement in perioperative care by enabling personalized risk stratification and optimized resource management for surgical patients.
Background: The Challenge of Prolonged Hospital Stays in GI Surgery
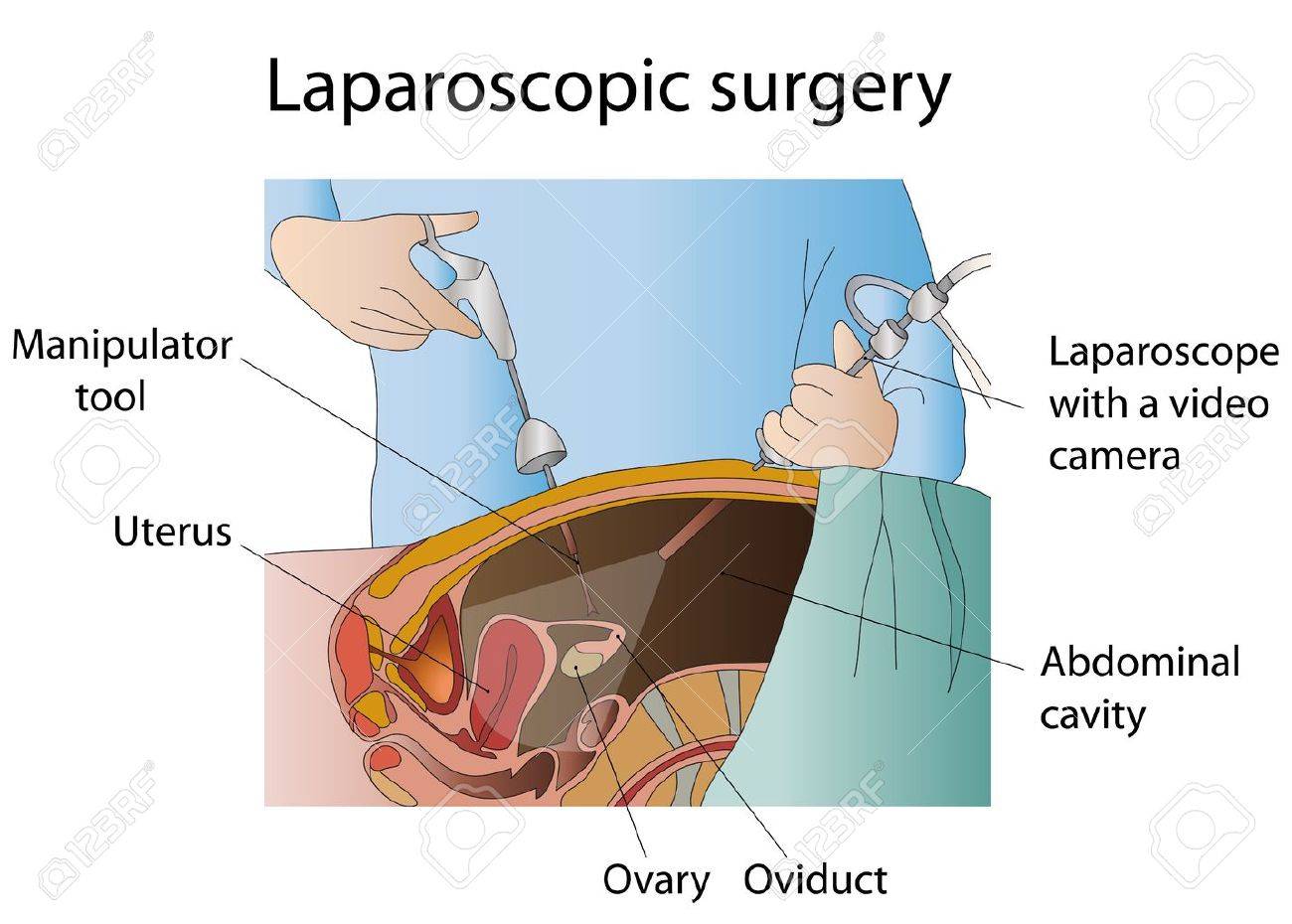
Minimally invasive laparoscopic GI surgery is increasingly preferred due to reduced postoperative pain and faster recovery compared with open surgery. However, some patients experience prolonged hospital stays, which can increase healthcare costs, resource utilization, and risk of complications such as infections or thromboembolism. Identifying these patients preoperatively or early post-surgery remains a clinical challenge.
Traditional risk scoring systems rely on limited clinical variables and often fail to capture complex interactions affecting recovery time. This gap has driven exploration of machine learning (ML) approaches for more accurate and dynamic predictions.
Development and Validation of the ML Prediction Model
The study utilized data from the FDP-PONV trial — originally focused on postoperative nausea and vomiting — to perform a secondary analysis targeting LOS prediction. Researchers applied advanced ML algorithms to integrate a broad range of perioperative variables, including patient demographics, comorbidities, surgical factors, and intraoperative data.
Key features of the model include:
- Multifactorial input: Incorporates clinical, surgical, and anesthetic variables.
- Nonlinear pattern recognition: Captures complex interactions beyond traditional linear models.
- Performance metrics: Demonstrated superior predictive accuracy compared to conventional statistical models.
- Validation: The model was internally validated within the trial dataset, showing robust discrimination and calibration for identifying patients likely to have prolonged LOS.
Clinical Implications
This ML model holds potential to transform perioperative management by:
- Early identification of high-risk patients: Allowing tailored interventions such as enhanced monitoring, targeted physiotherapy, or preemptive complication prevention.
- Optimizing hospital resource allocation: Anticipating bed occupancy to improve scheduling and reduce bottlenecks.
- Supporting shared decision-making: Informing surgeons and patients about expected recovery trajectories.
- Reducing postoperative complications: By enabling proactive management based on predicted risk profiles.
Broader Context of AI in Surgical Care
The application of ML in predicting surgical outcomes is rapidly expanding across various domains. Recent studies demonstrate ML models outperform traditional scoring systems in predicting surgical site infections, anastomotic leaks, and readmissions after GI and bariatric surgery. For example, the ES-Firm-Prev ratio was identified as a key predictor for infections, while tree-based models successfully forecast multiple postoperative complications simultaneously.
Moreover, clinical implementation of AI-based decision support tools for colorectal cancer surgery has shown promise in real-world settings, highlighting the feasibility of integrating such models into routine surgical workflows.
Future Directions and Challenges
Despite promising results, key challenges remain before widespread clinical adoption:
- External validation: The model requires testing across diverse patient populations and healthcare settings to ensure generalizability.
- Interpretability: Enhancing transparency of ML predictions to facilitate clinician trust and understanding.
- Integration: Seamless embedding into electronic health records and surgical planning systems.
- Ethical considerations: Addressing bias, patient privacy, and informed consent in AI-driven care.
Conclusion
The development of a machine learning-based model to predict prolonged length of stay after laparoscopic gastrointestinal surgery marks a substantial step forward in precision surgical care. By enabling early risk identification and personalized management, this innovation promises to improve patient outcomes, optimize healthcare resources, and reduce costs. Continued validation and integration efforts will be essential to realize the full potential of AI in surgical practice.
Relevant Image Descriptions:
- Graphical model flowchart illustrating the machine learning algorithm integrating perioperative variables to predict prolonged LOS after laparoscopic GI surgery.
- Visual representation of laparoscopic surgery, highlighting minimally invasive instruments and patient recovery context.
- Data analytics dashboard screenshot showing risk stratification outputs for individual patients derived from ML predictions.
These images provide visual context for the technology, clinical setting, and application of the predictive model.
This article synthesizes recent research findings and contextualizes their impact on surgical care, drawing from multiple academic and clinical sources.



